Let's Talk Breast Cancer Reconstruction
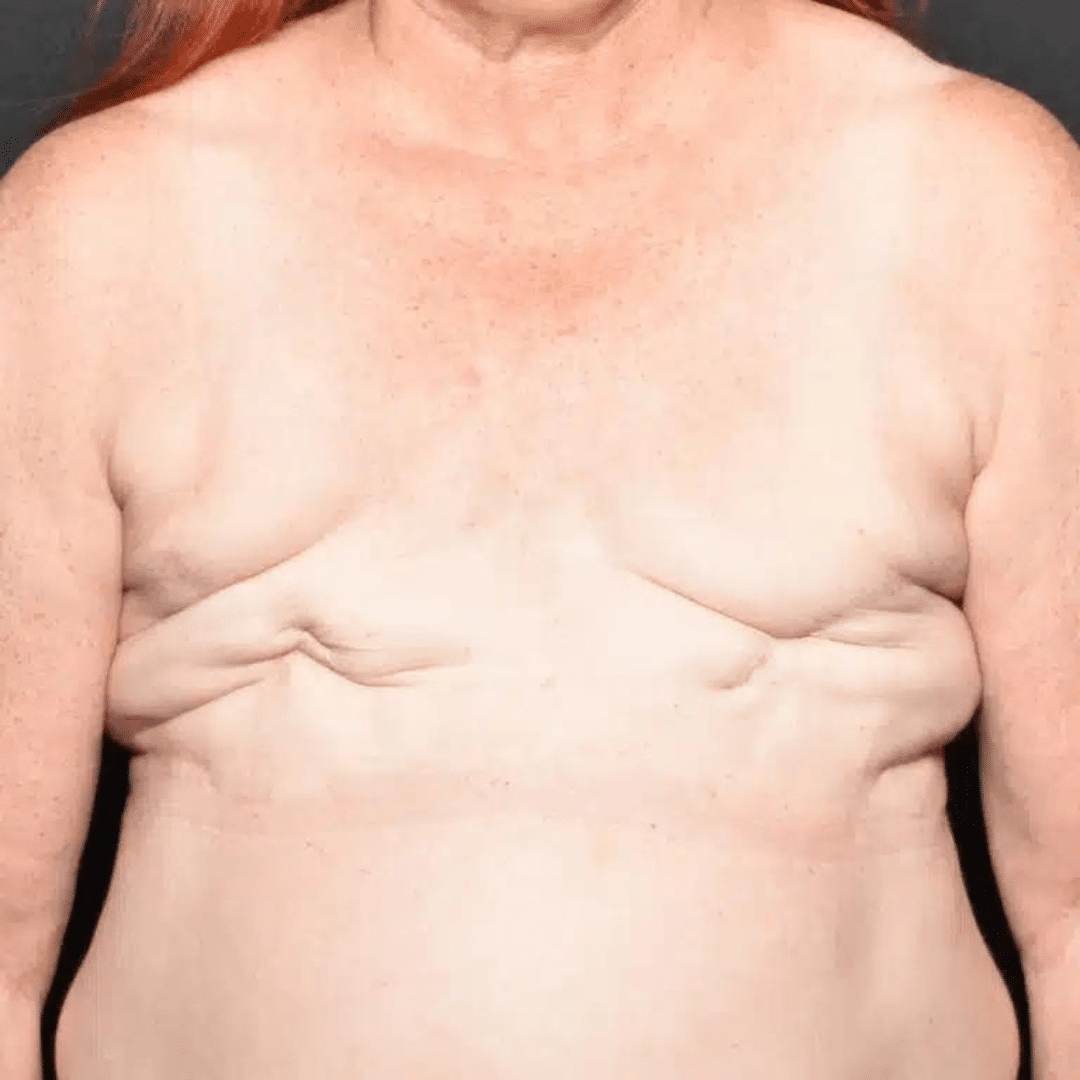
Dr. Elisa Burgess is highly committed to providing exemplary breast cancer reconstruction in a caring and compassionate manner. Dr. Burgess and her staff strive to offer exceptional care to all patients in a comfortable and friendly office setting. Breast Cancer reconstruction is a specialized group of surgical procedures which recreate the breast, following a mastectomy or lumpectomy.
There are several options to recreate the breast. Dr. Burgess guides her patients towards the best option for their indiviidual situation, with optimal outcome. Reconstructed breasts will look different from your natural breast, but they can look very nice and natural in clothing. Below is a general overview of breast cancer reconstruction and the possible options available in our clinic.
Implant Reconstruction:
Tissue Expanders:
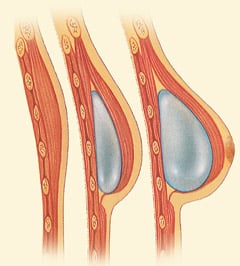
During mastectomy, or a later date, tissue expanders can be placed above the muscle (prepectoral) or under the muscle (subpectoral). The prepectoral placement can decrease animation movement of the tissue expander when the pectoris muscle is flexed, so this may look like a more natural reconstruction. The tissue expander is a temporary implant that contains a port within its shell. This port allows for adding more saline or air. Once the mastectomy incision has healed, to expand or fill the tissue expander. This process is known as expansion. Expansions normally start several weeks after surgery and occur every two weeks until you have reached your goal.
During a quick, in-office procedure, Dr. Burgess or her nurses will use a very fine needle to place about 50mL of saline or air into the port of your tissue expander, through a numb area on your chest. The pectoralis muscle may feel tight and uncomfortable that evening. Each patient has their own expansion schedule that can work around chemotherapy appointments, and their personal life. The number of required expansions is very patient-specific. Your final expanded volume depends on your individual goals.
Once you have reached a volume that you and Dr. Burgess feel is acceptable, you will undergo a surgery to remove the T.E and replace it with a silicone or saline implant.
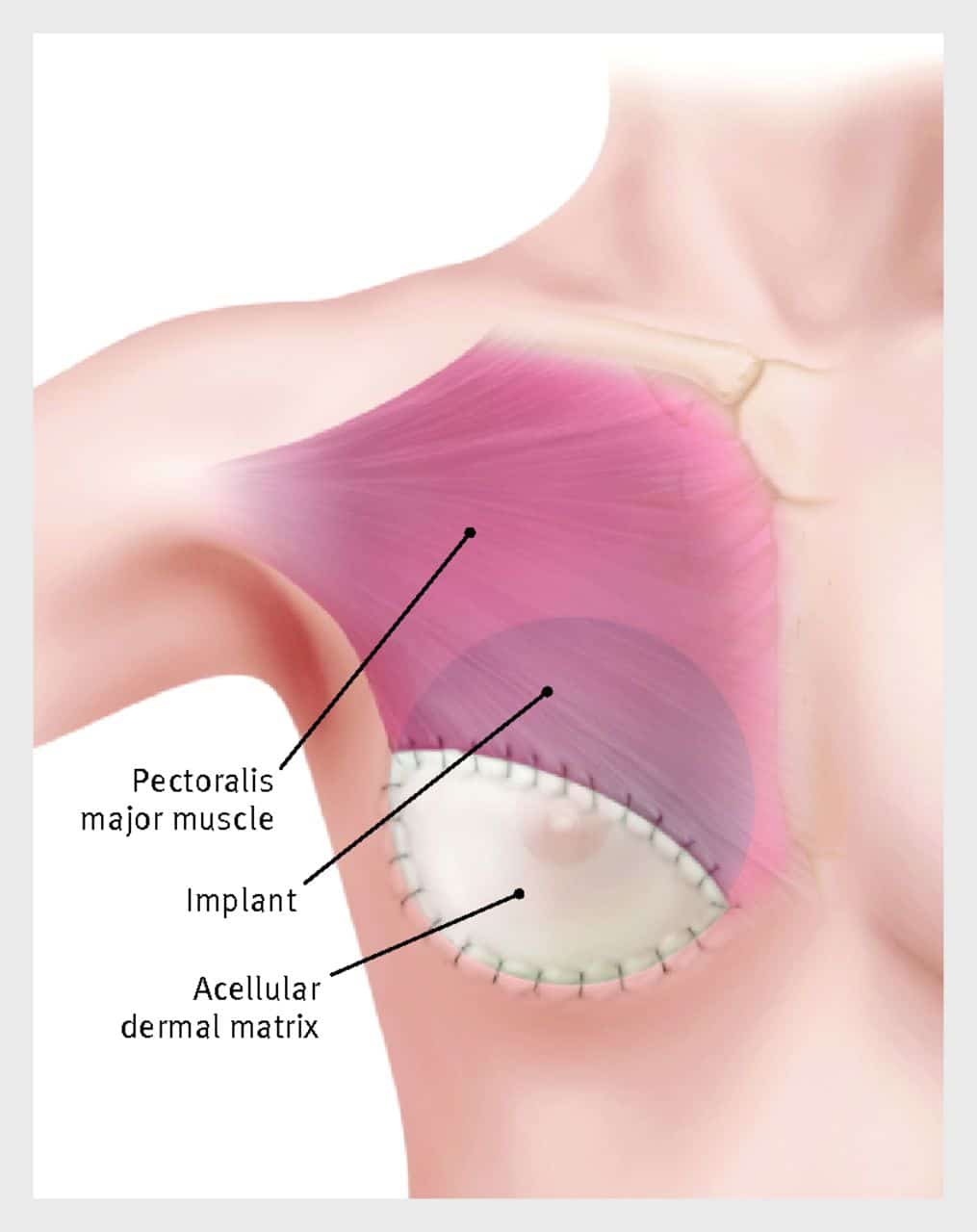
Acellular Dermal Matrix (ADMs):
After mastectomy, remaining tissue over the chest wall may be thin. The natural anatomy of the pectoralis muscle may not be adequate coverage for the implant. In this case, An Acellular Dermal Matrix (ADM) may be employed to provide lower pole for better support and coverage. An ADM is often a human cadaveric or porcine product that's utilized at the time of tissue expander placement.
The ADM is sewn into the pectoralis muscle, allowing for greater support in the lower breast pole, while supporting the tissue expander and eventually, the implant. It can provide a natural shape or “hang” to the breast. ADMs also support cellular growth and healing, while providing stabilization of the implant. It is possible that the T.E or implant could be placed on top of the muscle. However, it would typically be wrapped in a large piece of ADM.
Direct to implant:
Direct-to-implant reconstruction surgeries are performed at the time of mastectomy. They require the general surgeon and the plastic surgeon working in sync for part of the same procedure. Patients who have sufficient breast skin remaining after mastectomy may be well suited for direct-to-implant breast reconstruction. While direct-to-implant method avoids use of tissue expanders, secondary procedures may be preferred to improve symmetry or breast size. Unless the initial mastectomy was done using a nipple-sparing approach, most women proceed with reconstruction of the nipple and areola.

Flap Reconstruction:
Latissimus Dorsi Flap:
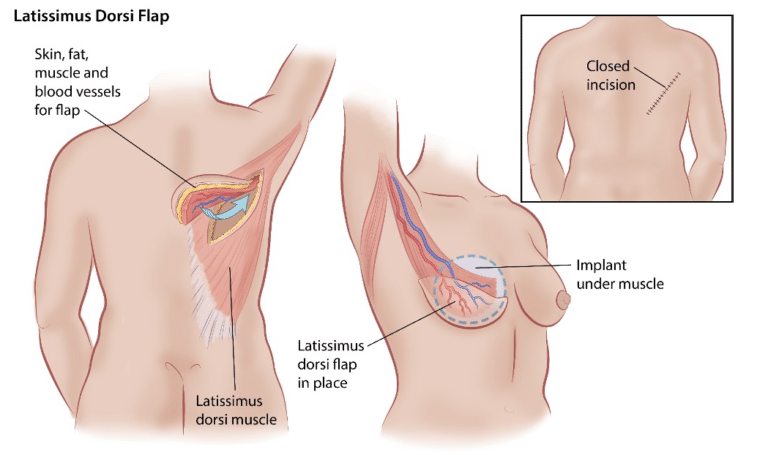
Another option for some is to reconstruct the breast using their own skin, tissue and latissimus muscle taken from the back and tunneling it to the breast area. This surgery is a favorable procedure for those that have undergone radiation and need fresh tissue to the chest. This is a major surgical procedure that can take 4-5 hours. Most women require several weeks off of work and should not work out vigorously for 8 weeks. Some patients require a T.E for additional volume, which is replaced with a permanent implant once the process is complete. Patients can expect a scar on the mid-back/shoulder area.
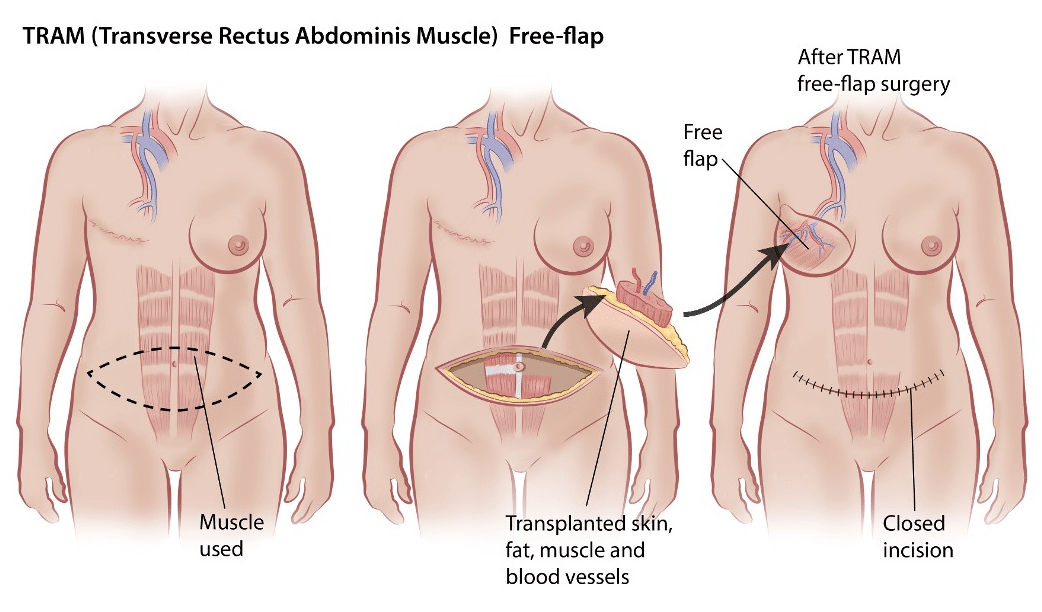
TRAM Flap:
TRAM (transverse rectus abdominis muscle) is a major surgical procedure. It involves using your own abdominal skin, fat and muscle to create and contour one or both breasts. This surgery can be upwards of 12 hours of surgical time and a 2-4 day hospital stay. The recovery from this surgery, as compared to the tissue expander procedure, is a greater length of time. With all reconstruction options, your surgeon will help guide you. This surgery is best for women who have some excess abdominal fat.
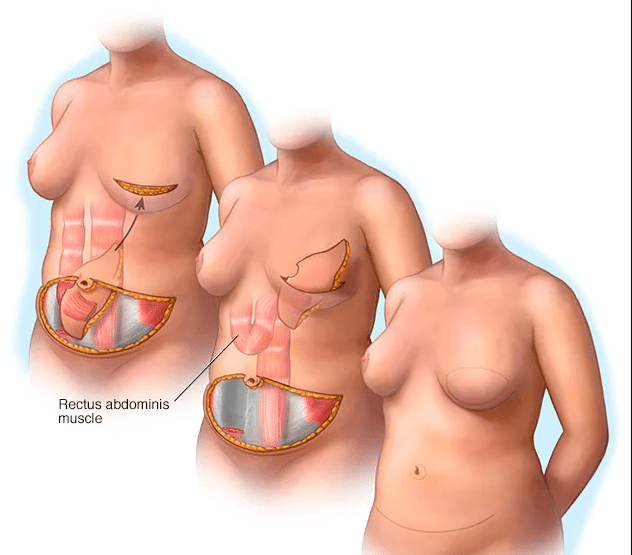
Here, the TRAM with fat and skin, is partially released and lifted up to form a new breast. Since your surgeon is harvesting this tissue from your abdomen, you also will end up with a tummy tuck. However, the abdominal wall will be reconstructed as well, usually with a piece of mesh or ADM. It is important to remember that this surgery will involve a scar across your lower abdomen and breast area. It is possible you will have some abdominal muscle weakness after this surgery.
Since your new breasts are created from your own tissue, they may feel natural. However, the skin sensation and coloring will be different. This is because the skin and tissue came from a different area of the body. Keep in mind that only certain patients are good candidates for the TRAM flap surgery.
DIEP Flap and Muscle SparingTRAM:
The DIEP Flap and muscle sparing tram types of breast reconstruction uses your own skin and fat to recreate the breast from the abdominal area.In this microsurgical procedure, blood vessels known as the deep inferior epigastric perforators, (DIEP) along with skin and fat are removed from the abdomen and relocated to the chest to create breasts. This type of flap surgery leaves the abdominal muscles intact. However, due to the complexity of this surgery, there are few facilities that offer the DIEP technique. Dr. Burgess does not routinely perform them but would be happy to refer you to a surgeon who does.
Lumpectomy and Breast Reduction:
Sometimes a breast reduction may be an option for larger breasted women who have been diagnosed with breast cancer. The mass is removed at the same time as the breast reduction. Many factors are considered, such as specific cancer diagnosis, stage, tumor location, breast size, treatment modalities and personal goals.
Following lumpectomy, a breast reduction will remove excess breast and fatty tissue in one or both breasts. This will make them smaller, lifted and more proportional to your body. Your size, anatomy and tumor location will dictate what type of surgical approach your plastic surgeon may use.
The Refinements:
We perform fat grafting in conjunction with other methods of reconstruction. Dr. Burgess will remove fat from another part of her body (i.e. stomach or thighs) and place back into flatter areas of the reconstructed breasts to create better fullness.
Once your breast reconstruction is complete, you may consider undergoing nipple reconstruction. This usually occurs at least three months after your final implant placement or muscle flap surgery. However, nipple reconstruction may be done much later, depending on patient preference.
Nipple reconstruction is a quick day surgery which uses your own tissue on the breast to create a nipple. The reconstructed nipple has projection, but no feeling or function. The areola is created by bringing in skin from another area of the body as a skin graft and then covering the nipple areolar complex with a protective dressing for about 5-6 days. Once this dressing is removed care must be taken to not injure them. Patients should avoid vigorous exercise for about one month. Most patients do not require much time off of work, usually only a few days.
Some women chose to only have a mastectomy to the affected or cancerous breast. This is known as a one-sided or unilateral mastectomy. To create symmetry between the reconstructed breast and the natural breast, patients often require surgery to the unaffected side. The type of surgery is patient-specific. Some smaller breasted women may require an augmentation, or implant to the natural breast, while some women may only need a breast lift. Others still may need a breast reduction to the non-cancerous breast if they are naturally very large breasted. Surgery to create symmetry is normally done at the time your final implant is placed to your reconstructed side, or after you have healed from your muscle flap surgery. With unilateral reconstruction there is no firm time frame for surgery to create symmetry.
The entire reconstruction process can take around one year to complete. Each patient has their own reconstruction timetable, with independent factors, such as chemotherapy, radiation or personal and family agendas that may affect surgery scheduling. Breast reconstruction is usually a staged process, to allow for healing, settling of the new breasts or implants and mental adjustment to your new look. Because breast cancer reconstruction is an elective procedure, patients should be in good overall health.
There are many support groups available to those with breast cancer, breast cancer survivors and their families. For more information, please click below.
Dr. Burgess and her staff have been incredibly competent and caring during my breast cancer reconstruction. Dr. Burgess came highly recommended by my surgical oncologist and I have been nothing but happy with the care I have received. - N.G.
Schedule a Consultation with Dr. Burgess
If you have questions regarding reconstruction procedure, do not hesitate any longer to schedule a consultation with Dr. Burgess. You can call 503-699-6464 and reach our office today. You can also submit an online contact form and we will get back to you at our earliest convenience.